
Improving Immunisation Uptake Team Initiative
In July 2018, SCW received additional funding (initially as a time-limited pilot) to develop an initiative to reduce inequalities in vaccination access and variation in childhood immunisation uptake across the Thames Valley Child Health Information Services (CHIS) area.
NHS England (NHSE) had previously commissioned a health inequalities project in 2017. This demonstrated improved outcomes when health inequalities nurses worked closely with CHIS.
After evaluating this project, commissioners recognised the need to better engage with GP practice colleagues. They saw how supportive discussions driven by data and intelligence from CHIS led to improved management and processes.
A further one-year pilot was initiated to allow the benefits of this combined clinician and CHIS resource approach to be further developed and systematically evaluated. This pilot commenced in July 2018 and the Improving Immunisation Uptake (IIU) team was set up to lead the project, including for the first time, clinicians working within CHIS. A blended team approach was taken, ensuring that clinicians were supported by a specialist data quality lead who had extensive experience in CHIS.
Uptake of the IIU team service was widespread across the Thames Valley. In some cases, it did take several months of contact between the IIU team and practices to secure their engagement.
Securing the engagement of underperforming GP practices, proved to be one of the key challenges of the pilot project as they were initially reluctant to be involved. The vast majority of practices however have engaged with the IIU team since the outset of the IIU initiative.
The objective of the IIU team initiative was to utilise CHIS GP level data and clinical input to improve vaccination uptake in 0-5-year-olds, with a particular focus on under-served children and communities in the Thames Valley.
Pilot project approach and methodology
The IIU team initiative used several approaches to deliver its objective. These were based on the lessons learned and outcomes achieved from the original commissioner-led health inequalities nurse project.
(See right)
Methodology
The first task for the IIU team in July 2018, was to systematically determine which of the Thames Valley GP Practices should be given priority for the IIU team to commence working with. To achieve this, a data report was produced ranking Thames Valley GP Practices according to their childhood immunisation uptake performance.
The rankings produced by this report were based on percentage uptake of all 0-5-year-old childhood immunisations, routinely given as part of the current national childhood immunisation schedule. The 20 lowest performing practices identified by the report, were given priority for intervention by the IIU team. Some work was also initiated with other practices identified on the list.
This report was run monthly throughout the IIU initiative. This enabled the review and monitoring of trends or changes within the 0-5-year immunisation uptake across the Thames Valley.
In parallel with targeting support and intervention on those GP Practices systematically identified as having low immunisation uptake rates, NHSEI also highlighted geographic areas within Thames Valley where they wanted intervention and support to be focused, such as underserved children and communities.
The IIU team worked closely with stakeholders and ensured alignment to relevant Primary Care initiatives in the areas identified, to ensure a joined-up collaborative approach.
Service delivery model
Graphic image (right) shows the circular relationship: - CHIS extracts immunisation data from GP - CHIS analyst cleanses data - Clinician reviews data - GP vaccinates children identified as missing immunisations -
The IIU team initiative commenced in July 2018 and was staffed through the creation of three new fixed-term posts. These posts comprised 1.6 WTE IIU team clinicians to which Health Visitors/Practice Nurses with a substantial immunisation background were recruited and 1 WTE data analyst/facilitator.
This service model was deployed to enable dedicated clinical input to work hand in hand with CHIS experience and expertise, thus providing the clinicians with greater data support, insight and intelligence. The data analyst/facilitator role ensured clinicians worked only with a fully cleansed data set from the operational CHIS team. This provided a list of children still resident and registered who were missing immunisations for each GP Practice under consideration. The data analyst/facilitator also addressed data quality issues.
This approach provided a robust analysis of children missing immunisations, with a particular focus on the 0-5-year-old population. It also provided a failsafe ensuring all children missing immunisations were promptly identified and followed up. The anticipated outcomes of the approach were to reduce the variation in immunisation uptake rates between GP practices and reduce the number of children missing immunisations within the Thames Valley.
To find out more about the work we do to support improving immunisation uptake, contact the team on scwcsu.improvingimmsuptake@nhs.net or 0300 561 1855.
Project governance and outputs
Project governance
The initial project governance was set up as below:
Action | By whom | Frequency |
|---|---|---|
Project delivery management | SCW-CHIS | 1 year |
Project performance management | NHSE | Monthly / quarterly |
Attendance and contribution to performance and working group meetings | SCW - CHIS | As agreed with NHSE |
Provide quantitative and summary activity report | SCW - CHIS | Monthly |
Provide recurring performance reports at practice level | SCW - CHIS | Quarterly |
Escalate concerns to commissioners e.g. barriers, stakeholder non-repsonders | SCW - CHIS | Timely |
Project outputs
Initially, SCW’s CHIS and IIU team, produced a baseline immunisation data dashboard to facilitate:
- focus on reducing variation between practices
- focus on priority areas e.g. geographic or low performing CCG’s
- performance metrics at practice, CCG, PCN and LA levels
- providing quarterly reports and narratives
- support commissioner initiatives with data for specific projects
As the service developed additional outputs were produced. One of these involved the IIU team providing training to practice staff. The IIU initiative found sufficient skilled and informed administrative resources were vital to improving immunisation uptake rates. GP practice administrative staff often work in isolation and providing group training sessions helped facilitate immunisation leads to network and share good practice.
Another of the agreed outputs from the IIU initiative was for the team to produce an updated immunisation toolkit for Primary Care, drawing on the learning achieved during the pilot. This was produced in May 2019 and has proven a useful tool for practices, in conjunction with practical support and guidance from the IIU team.
Feedback from GPs
Thematic analysis of feedback received from practices enabled the IIU team to:
- ensure targeted support was provided to improve immunisation uptake rates in the short term. And empower practices to develop their own strategies and processes to achieve long-term and sustainable high vaccination uptake rates, which meet or exceed current targets.
- demonstrate the real outcomes achieved by practices, due to the direct support provided by the IIU team. These outcomes assisted practices to achieve key targets for vaccinations, alongside reducing variation in immunisation uptake rates across the Thames Valley region.
- to review/plan/allocate internal resources to ensure the most appropriate support/resource is put in place for every practice. This included clinical advice and assistance with administration issues/training, data and/or processes.
Lessons learned
Many key lessons were learned from the IIU pilot project, for both primary care colleagues and the IIU team itself.
Ongoing facilitation of change management was crucial.
Practices needed regular follow up and robust action planning to support them with making the changes needed to increase their immunisation uptake rates and adopt a whole practice approach.
Immunisation processes were often not reviewed regularly or weren’t in place.
IIU team support enabled practices to draw up clear processes so that all staff (admin/clinical/managerial) had an appropriate level of understanding as to how immunisation worked in their practice. This ensured a consistent and collaborative whole practice approach. It also enabled new staff members (many of whom were not provided with training previously and had to learn on-the-job), to familiarise themselves with key processes as part of their induction. This was important as high staff turnover in practices is common.
Many practices didn’t have a clinical/admin immunisations lead.
Even in practices with a named lead, their role and responsibilities were often not clearly defined and/or agreed upon. This meant that there was little governance and/or overview of immunisation processes within the practice, with many Practice Nurse’s immunising only with a narrow clinical focus.
There was little collaborative working between clinical and admin staff (who often were the first point of contact for parents) with staff unsure of how to escalate immunisation issues.
Many Practice Nurses (and some Practice Managers) were unaware of their immunisation uptake rates and how robust processes (such as new registrations), could help improve these.
Key practice staff had no real understanding and overview of how immunisations could be increased and improvements made through adopting simple changes to immunisation practice and administration. The IIU team worked with practices to support them in adopting a whole practice approach between admin and clinical staff. This ensured robust processes were in place to ensure good communication, follow up and monitoring of immunisations. A key outcome from this was that often the Practice Nurse would continue to act as the clinical immunisation lead, supported by a named admin immunisation lead.
Robust processes for obtaining immunisation histories were commonly not in place at most practices.
Data quality was adversely affected and staff were not actively following up children with missing immunisations/records. This, in turn, had a negative effect on uptake rates. The IIU team supported practices to review their registration processes to ensure histories were obtained.
Availability and flexibility of appointments for immunisations was a common challenge identified by both staff and parents.
This affected both the timeliness of immunisations (e.g. vaccines being given too early or too late) and also contributed to DNA’s, where parents couldn’t bring their children in at the pre-set times e.g. first thing in the morning.
Delivering vaccines too early was commonplace in some practices.
Where immunisations were being given too early, these were categorised in data reports as missing, impacting uptake rates.
The IIU team worked with both clinicians and admin staff, to ensure that they understood the importance of ensuring that immunisations were not given too early. They also initiated robust processes to facilitate the booking of appointments (often completed by admin/reception staff) to ensure this didn’t happen.
Sharing good practice across GPs, helped individual surgeries recognise where they could make improvements and the benefits that could be realised as a result.
The IIU team supported practices to reach out and network/buddy up with other local GP’s in their area. This enabled practices to share learning and provide peer-to-peer support.
This proved to be particularly beneficial for smaller practices with few members of staff and perhaps only one Practice Nurse.
Improving practices understanding of the role of CHIS and their processes/data requests.
Immunisation data should be returned electronically. Some practices were returning in paper form as they saw electronic returns as an additional burden to their workload, with little benefit to them.
The IIU team worked with practices to provide further clarification on data collection, which supported practices understanding of CHIS and ensured reports were completed correctly and in a timely manner
Several practices were sending their own immunisation invitation letters to parents but this was not documented anywhere.
In doing this, many practices were also duplicating letters already produced and sent by CHIS. Initially, some practices were reluctant to stop sending their own letters, but the vast majority discontinued this practice.
This has released additional admin time/capacity to focus on other initiatives related to immunisations, which are much more effective in increasing uptake rates. It has also helped reduce parental frustration at receiving multiple letters.
Data quality was a major ongoing issue for practices.
In particular, 'ghost patients' were commonplace on missing immunisation reports with no process in place to identify these, validate whether they were still living locally and then remove them. The fact that 'ghost patients' had not been de-registered had a significant impact on uptake rates for many practices.
The IIU team data lead and clinical staff, worked with practices to support them with data cleansing. This ensured that the missing immunisation reports gave an accurate overview of the children still requiring vaccination and didn’t include children who had left the practice/area.
The IIU team’s work with practices has encouraged them to explore how lessons learnt from improving childhood immunisation uptake rates can be applied to other important public health initiatives such as flu uptake rates, screening programmes and health checks.
During their work with practices, the IIU team encouraged teams to work collaboratively across PCNs to share and promote best practice and identify effective new ways of working e.g. digital/virtual offers.
Increasing primary care collaborative working also provides scope for a better overview of inequalities/variations in care across regions and systems, which can support improving health care outcomes for all. The IIU team’s work with practices provided an opportunity to gather intelligence that could be used to identify trends and emerging/long-standing issues that could affect uptake rates and outcomes locally, regionally and nationally.
End of project outputs
A number of additional outputs from the project helped shape the evolution of the IIU team service following the initial pilot.
- Evidence-based learning recommendations for GPs
- Clinical resources (GP toolkit / Top tips) for practices
- Project evaluation and recommendations for future IIU team service
- Increased and sustained uptake rates across the Thames Valley
- Immunisation capacity building and sustainment in practices
- Improved awareness of best practice to increase uptake rates
Project summary
During the IIU initiative, the team provided a wide range of direct support to practices in primary care. The pilot initiative demonstrated how the use of whole GP practice team meetings and continual engagement were key components for achieving sustained improvements in immunisation uptake rates.
Achieving sustained improvements in immunisation uptake rates, requires the correct skill mix of data quality and analytical skills, to ensure all necessary data cleansing and data quality work has been completed. Effective engagement with Primary Care is facilitated by combining this with clinicians who can work with the whole GP practice team. Empowering practice teams to improve their immunisation uptake performance and secure the engagement and commitment needed to implement the required system and process change, is vital to the success of the IIU initiative.
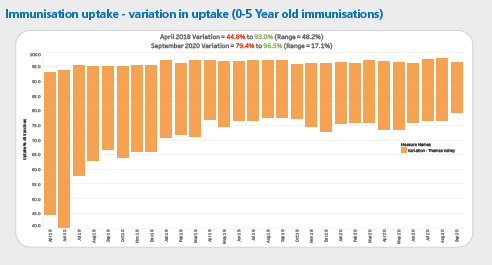
The pilot IIU initiative delivered a significant reduction in the variation of immunisation uptake across the Thames Valley and shows the overall increase in uptake of childhood immunisations. The graph below demonstrates the variation in immunisation uptake from April 2018 to September 2020 from x to y.
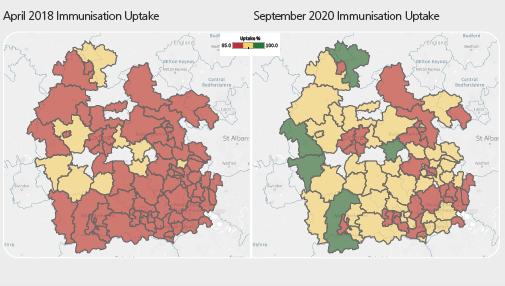
The heatmaps below, demonstrate the average uptake of each of the areas prior to the IIU team initiative and after.
Immunisation uptake - variation in uptake (0-5 year-old immunisations)
Thames Valley immunisation uptake - average by postcode area
Progress across the Thames Valley
The IIU team and commissioners set a key performance indicator for practices to increase their immunisation uptake rates to 80% or above.
As a result of the IIU team initiative, by the end of the pilot project great progress had been made across the Thames Valley (see below):
- Across the Thames Valley, 90.1% of practices were achieving over 85% immunisation uptake rates. 4.6% of these practices were achieving over 95% immunisation uptake rates
- Previously, 8 out of 24 practices in a targeted area in West Berks were achieving 80% immunisation uptake rates, this rose to 23 out of 24 practices. 5 of these practices then achieved 90% immunisation uptake rates
- The average immunisation uptake rate across a targeted area in West Berks increased from 74.9% to 86.8%
IIU team support during COVID-19
Despite the ongoing success of the IIU team service, the start of the Coronavirus pandemic in March 2020, led to a number of practices across the Thames Valley seeing an initial drop in their childhood immunisation uptake rates. The resulting challenge for the IIU team was to identify and address issues that were impacting on the uptake rates for childhood immunisations and practices’ capacity to deliver the national immunisation programme.
The IIU team worked in partnership with practices and parents to ensure the national childhood immunisation programme continued to be delivered during lockdown. The IIU team’s support included virtual face to face meetings, telephone calls and email contact with practices and parents. The IIU team contacted practices who had low uptake rates and worked with them to establish new ways of working and / or adapt current processes, so that they were able to continue providing immunisations.
A COVID 19 log was established, which enabled the IIU team to collate intelligence and escalate ongoing concerns directly to NHSEI during regular touchpoints. Many issues escalated to NHSEI were relevant at local, regional and national levels and were identified as a result of local intelligence gained by the IIU team e.g. Registering new births and the issues delays with this caused, such as timely vaccinations. The log also helped identify new ways of working, which meant good practice could be shared between areas / practices.
Due to the support provided by the IIU team, the following outcomes have been achieved:
- Increased use of online consulting and appointment booking for immunisations.
- Updating of practice websites to provide additional information for patients on key services such as immunisations and signposting to other forms of support.
- Practices and staff relocating to other premises to continue offering immunisation services, where a practice had been designated as a COVID-19 hub.
- Staff who were shielding were redeployed to review immunisation data and following up children with outstanding immunisations, either with parents directly or via practice nurses.
- Additional immunisation clinics were put in place due to spare capacity provided by some ’routine’ work being put on hold.
- Neighbouring practices shared vaccination staff to cover sickness / shielding or applied for additional funding for locum staff.
- Staff were redeployed from one area of work within a practice to another e.g. reception staff investigating and actioning children with outstanding immunisations. Staff reported that as parents were at home due to lockdown, contacting them was much easier.
- Working with parents to ensure that those having difficulty registering births, did not also face further challenges getting their child immunised.
- Parents were able to contact the IIU team for advice when they couldn’t contact their own practice.
- Practices reviewed their processes and adapted them where necessary.
- Communication between practices and parents improved.
- Key challenges affecting uptake rates at local and regional levels were escalated to NHSEI so that they could be addressed nationally.
- The IIU team also participated in virtual large scale statutory training for practice staff and wider healthcare professionals involved with immunisations.
- The IIU team worked in partnership with NHSE to develop guidance for practices on priorities during the pandemic.
During the initial phase of the pandemic, national figures for childhood immunisations fell. However, despite an initial drop in April, across the Thames Valley, rates were then maintained and / or increased. Many practices developed new ways of delivering key services such as vaccination programmes or adapted current processes during COVID-19. The IIU team continue to support practices during COVID-19.
The IIU team service today
Due to the success of the IIU initiative, it was recommissioned by NHSEI as an added element of the CHIS contract across the Thames Valley in September 2018.
Following review, the IIU team has further evolved and developed since September 2019 and now includes a clinical and team lead, a clinician, and a clinical data liaison lead.
They adapted their service model during COVID-19, to ensure the support provided to practices continued. New ways of working for the team were implemented e.g. Increased use of MS teams to provide remote support to practices, instead of face to face. This change to the way of working with practices has been very successful and has led to increased efficiency within the IIU team, by drastically reducing travel times to visit individual practices. This team has been able to provide increased support and resources to support a greater number of practices.
Practices have also seen the benefit of remote support via MS Teams. More staff members have been able to join meetings, either in the practice or from home (if they are shielding, working from home or self-isolating).
Uptake rates across the Thames Valley have continued to increase since the IIU team was made permanent,. Building on learning gained during the pilot IIU project the team adjusted in January 2020 to move focus from overall 0-5 year immunisation uptake to a focus on improving preschool booster rates (PSB). The team had identified a significant variation in uptake between the primary / 1 year immunisations and the preschool booster uptake. Many practices had a high uptake for their primary immunisations but a significantly lower uptake for their preschool booster.
The table below shows an 81% reduction in the number of practices across the TV under 80% uptake for PSB at the beginning of the year from January to October.
Month | Number |
|---|---|
January 2020 | 27 |
October 2020 | 5 |
Preschool booster uptake success in 2020
Percentage | January | November |
|---|---|---|
<80% | 27 practices | 5 practices |
80-84% | 48 practices | 33 practices |
85-89% | 59 practices | 69 practices |
90% | 74 practices | 97 practices |
All vaccine uptake immunisation success in 2020
Percentage | January | November |
|---|---|---|
<80% | 16 practices | 1 practice |
80-84% | 41 practices | 22 practices |
85-89% | 64 practices | 58 practices |
90% | 87 practices | 123 practices |
Due to the success of SCW’s IIU team, other areas have expressed an interest in the service, with the potential for it to be upscaled further across different regions.
The support of our colleagues, has been instrumental in the continued success of the IIU team and we are very grateful for their contributions to improving immunisation uptake rates across the Thames Valley and reducing variation across the area.
The IIU team would like to express their thanks to the following:
- Our commissioners - NHSEI
- Our colleagues in CHIS and the data informatics team
- Our colleagues in primary care
- Our colleagues in SCW
To find out more about the work we do to support improving immunisation uptake, contact the team on scwcsu.improvingimmsuptake@nhs.net or 0300 561 1855.


